Herpes zoster and post herpetic Neuralgia
Dr.NEAZA.A,
PHYSICIAN
ESI H, PEROORKADA
drneaza@hotmail.com
A 63-year-old woman presented in our OPD with
persistent pain and itching in the right T10 dermatome from just above the
thoracolumbar junction to the umbilicus. She gives history of episode of herpes
zoster in the same region one year earlier. She describes a severe, continuous,
burning pain lasting a few seconds, and intense hypersensitivity to tactile
stimulation.
On physical examination there are signs of
cutaneous scarring throughout the right T10 dermatome, with areas of
excoriation caused by scratching.
Post
herpetic neuralgia (PHN) is the most frequent chronic complication of herpes
zoster.
Herpes zoster (HZ), commonly called shingles,
is a distinctive syndrome caused by reactivation of varicella zoster virus
(VZV) in the dorsal root ganglion of sensory nerves. This reactivation occurs
when immunity to VZV declines because of aging or immunosuppression..
Historical
Perspective:
VZV is estimated to have been around for more
than 70 million years. It was initially named by Hippocrates; Herpein, meaning
to creep; zoster meaning girdle
(Greek). Shingles meaning belt, (Latin).
Not until 1940 was the etiology of the virus established. VZV was finally
isolated in 1952 by a Harvard Microbiologist. The
genome was first sequenced in 1986.
Epidemiology:
Varicella zoster virus (VZV) has a high level of infectivity and has a worldwide prevalence.
Incidence:
5-10 cases per 1000 persons. It is highest among individuals in the
sixth decade of life and beyond.
Following primary infection of the virus
(Varicella -chicken pox), it lies dormant until reactivated in later life.
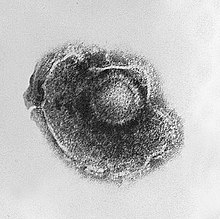 Varicella virus
Varicella virus
Pathophysiology:
Reactivation can occur
in the presence of stress, surgery, or injury. Following reactivation the virus
travels at a possible rate of 1.7-10mm per hour. Cutaneous vesicles develop in
48-96 hours. Hemorrhagic inflammation is characterized at the cellular level. Fibrosis
is noted at the dorsal root ganglion, nerve root and peripheral nerve upon
resolution of the acute stage.
Postherpetic neuralgia
is the nerve damage caused by herpes zoster. The damage causes nerves in the
affected dermatomic area of the skin to send abnormal
electrical signals to the brain. These signals may convey excruciating pain, and may persist or recur for
months, years, or for life.
Neuropathic pain is due
to altered gene expression in sensory dorsal root ganglia neurons. Following nerve damage, NaCl channel
accumulation causes hyperexcitability, and down regulation sensory neuron
specific, SNS1 channel and upregulation of brain type III and TRPV1 channels.
These changes contribute to increased NMDA glutamate receptor-dependent
excitability of spinal dorsal horn neurons and are restricted to the
ipsilateral (injured) side. A combination of these factors could contribute to
the neuropathic pain state of postherpetic neuralgia.
Clinical manifestations:
Prodromal symptoms may
include chills, fever, malaise, G.I. disturbance and paraesthesia or neuralgia
along the affected dermatome.
Red papules usually appear along the affected
dermatome within 3 days. The eruption of vesicles closely follows the maculopapular
rash. Vesicles usually dry up in an average of 7 days and scarring occurs at
the site.

Distribution: 50-60%
Thoracic, 10-20%Trigeminal, 10-20%Cervical, 5-10% Lumbar, and <5% Sacral. 99%
of all cases are unilateral and do not cross the midline unless there is
greater than one dermatome affected or dissemination has occurred.
Sensory disturbances face
Diagnosis and differential diagnosis:
If the rash has
appeared, identifying this disease requires only a visual examination, since
very few diseases produce unilateral vesicular lesion in a dermatomal pattern.
Herpes simplex virus (HSV) can occasionally produce a rash
in such a pattern (zosteriform herpes simplex). The Tzanck
smear is helpful for diagnosing
acute infection with a herpes virus, but does not distinguish between HSV and
VZV.
Coxsackie virus
infection also produce disseminated vesiculopapular lesion. Supportive
diagnostic virology and fluorescent staining of skin scrapings with monoclonal
antibodies ensure proper diagnosis.
Laboratory tests;
The most popular test detects VZV-specific IgM antibody
in blood; this appears only during chickenpox or shingles and not while the
virus is dormant. Lymph collected from a blister is
tested by polymerase chain reaction for
VZV DNA, or examined with an electron
microscope for virus particles. Viral culture and quantitative PCR are done with
samples of lesions on the skin, eyes, and lung.
To
assess host response immunofluorescent detection of antibodies to VZV membrane
antigens, fluorescent antibody to membrane antigen (FAMA) test and ELISA appears
to be most sensitive.
Complication:
Secondary bacterial
infection of the skin
Post herpetic neuralgia
is a condition of chronic pain following shingles. The neuralgia typically begins when the herpes zoster vesicles have crusted over and begun to heal.
Nervous system involvement cause many cranial neuropathies, polyneuritis, myelitis, or aseptic meningitis, partial facial paralysis (usually temporary), ear damage, or
encephalitis.
Trigeminal nerve involvement in herpes ophthalmicus
should be treated early and aggressively as it may lead to blindness.
Involvement of the tip of the nose in the zoster rash is a strong predictor of
herpes ophthalmicus.
Herpes of the geniculate ganglion presents with facial nerve palsy
causing Ramsay- Hunt syndrome
During pregnancy, first infections with VZV, causing chickenpox,
may lead to infection of the fetus and complications in the newborn, but
chronic infection or reactivation in shingles are not associated with fetal
infection.
There is a slightly
increased risk of developing cancer
after a shingles infection.
Treatment:
The aims of treatment
are to limit the severity and duration of pain,
shorten the duration of a shingles episode,
and reduce complications. Symptomatic treatment is often needed for the
complication of post herpetic neuralgia.
Antivirals:
Antiviral drugs may reduce the severity and duration
of shingles; however, they do not
prevent postherpetic neuralgia.
Of these drugs, acyclovir has been the standard treatment, but
drugs valaciclovir and famciclovir
demonstrate similar or superior efficacy and good safety and tolerability.
The drugs are used both for prevention and as therapy during the acute phase. Complications in immunocompromised individuals with shingles may be
reduced with intravenous acyclovir. In people who are at a high
risk for repeated attacks of shingles, five daily oral doses of acyclovir are
usually effective.
Analgesics:
People with mild to
moderate pain can be treated with analgesics.
Locally
applied topical agents
Aspirin
mixed into an appropriate solvent such as diethyl
ether may reduce pain.
Lidocaine skin patches
Once
the lesions have crusted over, capsaicin cream (Zostrix) can be used.
Calamine lotions
can be used on the rash or blisters.
Paracetamol or the non-steroidal anti-inflammatory drugs
and opioids including higher
dosages of codeine, tramadol, morphine or fentanyl are beneficial for pain relief.
Pain modification therapy:
Antidepressants:
Low dosages of tricyclic antidepressants, including amitriptyline,
are used for the deep aching pain. They do not eliminate the pain, but they may
make it easier to tolerate.
Other
antidepressants- venlafaxine, bupropion and selective
serotonin reuptake inhibitors also used in postherpetic neuralgia .
Anticonvulsants:
These agents are used to manage severe muscle
spasms and provide sedation in neuralgia. Phenytoin
and carbamazepine can lessen the pain associated with postherpetic neuralgia.
The medications stabilize abnormal electrical activity in the nervous system
caused by injured nerves
Gabapentin
and lamotrigine,
are generally tolerated better and can help control burning and pain in PHN.
Steroids:
Corticosteroids have
been recommended to help with acute pain but do not appear to decrease the risk
of long term pain.
Non-pharmacological treatments for post herpetic neuralgia:
Acupuncture.
Moxibustion: A traditional Chinese medicine therapy using
moxa.
Relaxation
techniques. These can include breathing exercises, visualization and
distraction.
Heat therapy.
Cold
therapy Cold packs can be used.
Transcutaneous
Electrical Nerve Stimulation. This involves the stimulation of peripheral nerve
endings by the delivery of electrical energy through the surface of the skin.
Spinal
cord stimulator. The electrical stimulation of the posterior spinal cord works
by activating supraspinal and spinal inhibitory pain mechanisms.
Prevention:
A live attenuated varicella vaccine (Oka) is
recommended for all children >1 year of age (up to 12 years of age) who have
not had chickenpox and for adults known to be seronegative for VZV.
A second
approach is to administer varicella-zoster immune globulin (VZIG) to
individuals who are susceptible, are at high risk for developing complications
of varicella, and have had a significant exposure
Lastly,
antiviral therapy can be given as prophylaxis to individuals at high risk who
are ineligible for vaccine or who are beyond the 96-h window after direct
contact.
Prognosis:
The rash and pain
usually subside within three to five weeks.
One in five people
develop post herpetic neuralgia, which is often difficult to manage.
In some people, shingles
can reactivate presenting as zoster
sine herpete: pain radiating along the path of a single spinal nerve, but
without an accompanying rash.
Bibliography
1.
Longo, Fauci, Kasper et al ; Harrison’s principles of internal medicine 18th
edition 180:1462,2012.
2. Kantaria SM.Bilateral
asymmetrical herpes zoster, Indian Dermatology online j2015;6:236.
3.
Am Fam Physician. 2000 Apr 15;61(8):2437-2444
(copy of article published in JIMOA vol111 issue 1 sep 2015)








